Periodontal Disease
There are two classifications of periodontal diseases based on the severity of the disease: gingivitis and periodontitis. Gingivitis is a gum infection caused by bacteria and plaque, it affects only the gums and is reversible. Gingivitis, however, may lead to more serious harmful forms of periodontal disease called periodontitis. Periodontitis is one of the main contributors to premature tooth loss.
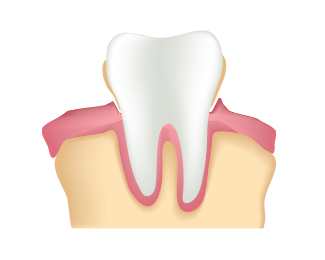
You may have periodontal disease and have none of these symptoms. This is where regular dental checkups, your dentist and hygienist play a pivotal role in diagnosis and prevention. Periodontal disease is an infection of the gums and supporting bone as a result of high levels of bacteria that start a release of tissue-destroying enzymes. There is a part of your gum that is actually not attached to your teeth. It is a shallow v-shaped crevice between the tooth and gum and is called a sulcus. Gum disease attacks the area within the sulcus just below the gum line. The disease causes a breakdown of the attachment of the tooth and its supporting tissues. As the disease progresses the tissues are damaged and the sulcus now becomes a pocket. Typically, the more severe the disease or infection, the greater the pocket depth. Treatment is aimed at stopping further damage and reversing the progression of the disease.
To help further educate our patients on the topic of gum disease, we’ve provided the articles below.
Are your gums in a healthy state or are you suffering from gum disease? This is something that you need to know the answer to, but probably don’t. However, the CDC reports that 47% of adults in the US suffer from gum disease, making it one of the most common oral health problems in the US.
Unless you have been diagnosed by your dentist, you probably don’t know if you are suffering from some form of gum disease (also known as periodontal disease) or not. The reason for this, is that periodontal disease does not present many signs or symptoms. The few you can look for include unexplained bleeding while brushing or flossing, and your gums appearing bright red and inflamed.

If you notice either of the above signs, you should schedule a dental appointment ASAP. Your dentist’s office will have specialized tools to determine the health of your gums. Additionally, these tools will determine how far your gum disease has developed and what treatment is necessary. The earlier you catch gum disease, the better off you will be, as, if you let gum disease develop too far, it will not be able to be fully cured. Your dentist will be able to put together a personalized treatment plan to improve the overall health and wellness of your gums. Please note that a treatment plan may include the work of a periodontist.
Determining if you have periodontal disease, and receiving necessary treatment, is critical for your oral health. Along with this, gum disease has been associated with many other diseases including:
- Cardiovascular Disease
- Rheumatoid Arthritis (RA)
- Diabetes

As with any health issues, you are better off preventing periodontal disease from ever forming. Gum disease can be usually avoided by following instructions below:
- Brush twice per day for two minutes
- Floss daily
- Brush your tongue, roof of your mouth, and gums
- Use mouthwash
If gum disease does develop, there is treatment available, such as scaling and root planing, also known as a deep cleaning.
Nearly half of all Americans suffer from periodontal disease. Periodontal disease, also known as gum disease, is an infection that resides below the gum line. Not only can periodontal disease lead to tooth loss, but there are also many serious ailments with known connections to this disease, including cancer, heart disease, stroke, diabetes, and others. The importance of treating periodontal disease can’t be overstated.
Aerni Dental is proud to now offer LANAP® protocol for periodontal disease treatment.
What is LANAP?
LANAP stands for Laser Assisted New Attachment Procedure. As the name implies, it is a laser-based treatment for gum disease, which allows for the gums to be treated without the need for cutting or sutures. With the PerioLase® MVP-7™ laser, Dr. Aerni is able to vaporize the bacteria hiding deep within gum pockets, removing infection below the gum line. Compared to traditional gum surgery, the LANAP procedure is less invasive, and patients report less discomfort both during and after treatment. The LANAP protocol is the highest standard of care available in the world for the treatment of periodontal disease. Often we can save teeth that have previously been deemed hopeless, and regenerate the bone around the tooth.
LANAP treatment is the first and only laser protocol awarded FDA clearance for True Periodontal Regeneration. Its effectiveness is backed by both domestic and international studies. LANAP protocol can save teeth that would otherwise require extraction by promoting bone regeneration around the tooth. LANAP treatment saves teeth, reduces pocket depth, and regenerates bone growth to achieve optimum periodontal health.
LANAP treatment is the ONLY FDA-cleared protocol for full mouth True Periodontal Regeneration, the gold standard of gum disease treatment! It is also the ONLY laser with the science, research, and human histological studies to PROVE its claims! No matter which clinician you decide to get laser treatment from, be sure that your doctors are LANAP Certified and using the PerioLase® MVP- 7™. The LANAP protocol CANNOT be performed using other lasers.
Right now, there are millions of Americans living with gum disease; however, only a small percentage of this number will seek professional treatment—either from fear of treatment or lack of understanding of the serious consequences of untreated gum disease. Research has linked gum disease to a variety of health complications including diabetes, heart disease, pancreatic cancer, and low birth weight.
Until recently, treatments for gum disease have been invasive and painful. Proper treatment meant either dental surgery to cut and remove affected gums or extracting teeth and replacing them with dentures or dental implants. Recent advances in dental technology have provided a more precise alternative with the PerioLase® MV P-7™ and the LANAP® protocol.
The LANAP procedure utilizes the highly specialized PerioLase MVP-7 laser to provide a less invasive, more acute treatment for gum disease. The protocol targets and kills the bacteria that cause gum disease, without harming healthy tissue. LANAP protocol treats gum disease without the pain, gum line recession, or increased sensitivity traditionally associated with periodontal surgery. Additionally, LANAP treatment offers more predictable long-term results.
What are the benefits of LANAP (over traditional gum treatments)?
- Quicker Healing – As LANAP is a minimally-invasive treatment, the body is able to recover more quickly.
- Less Discomfort – There is less pain and discomfort both during and after LANAP treatment.
- No Incisions or Sutures – Treatment with LANAP eliminates the bacterial infection without the need for cutting and sutures.
- Minimal Recovery Time – A less-invasive treatment means patients can typically return to their daily routine much faster.
- Less Risk of Gum Recession – Since no cutting is required, patients are less likely to experience gum recession with the LANAP procedure.
- Less Gum Inflammation and Bleeding – The inflammatory bacteria can be targeted by the PerioLase MVP-7 laser without harming healthy tissue.
- Avoid Tooth Loss – Severe cases of periodontal disease can result in loss of teeth, but LANAP treatment has proven to be able to help many of these patients save their teeth. Keeping your natural teeth has been shown to be linked to having a longer lifespan!
- Safer for patients with Health Concerns – For those with health concerns such as HIV, diabetes, hemophilia, or on medications such as Plavix or aspirin, LANAP has shown to be a safe gum disease treatment option.
How is LANAP different from traditional gum surgery?
If you have been told that you have periodontal disease and surgery will be required, it is important to know the difference between traditional gum surgery, which utilizes a scalpel and sutures, and laser surgery.
Traditional surgery typically utilizes a scalpel so that the doctor can reflect the gum tissue back for visibility and to clean the pocket and reduce the pocket depth. The pocket depth is reduced by cutting away tissue. In many cases, the additional use of bone grafting or membrane materials will be needed in order to achieve reattachment of the gum tissue to the root surface of the tooth. Although in some cases the only way to treat the patient is by traditional surgery the vast majority of patients that we see opt for the less invasive and more comfortable LANAP protocol.
LANAP surgery does not require the use of a blade, or sutures. It is a minimally invasive surgery that results in very little recession and pain for the patient. The laser operates at a wavelength that can tell the difference between the diseased tissue and the healthy tissue. This means that the laser is extremely safe and selective when being used in surgery. For the first time, we can remove the diseased tissue and bacteria from your gums without harming, cutting, or removing healthy tissue!
Key differences between LANAP and traditional gum surgery, include:
Less Pain - Traditional surgery can be fairly painful and require pain medication and downtime. Many patients opt for dental implants to avoid the pain involved in gum surgery. The LANAP protocol involves much less discomfort. There is almost never a need to prescribe pain medication and the patients can usually go right back to work and move on with their daily routine.
Less Gum Recession After Surgery - Because traditional surgery requires the use of a blade there is no getting away from the gum line being reduced. The question is how much. Traditional surgery can result in lowering the gum line anywhere from 2-4 mm all the way to 10-15mm. LANAP treatment is much less invasive and more selective in the tissue that it cuts. This results in little to no recession of the gum line. This is a very important difference because recession can lead to a number of aesthetic problems for the patient, and cause the teeth to become very sensitive to cold and hot temperatures.
Shorter Healing Time - The healing time for LANAP treatment is much faster because it is an advanced technology that is less invasive than scalpel surgery. The laser kills the bacteria in your pockets resulting in a reduction of inflammation and healthier tissue.
More Predictable Long-term results - Although we can have fantastic results long-term with both treatments, LANAP treatment is far more predictable when it comes to bone regeneration and connective reattachment of the tissue. The laser stimulates the bone that surrounds the root of the tooth and has been proven to encourage regeneration, often saving teeth that would have previously been extracted. Many times we can reverse the effects of periodontal disease and the patient will get better and better as time goes on.
What should I expect from my LANAP procedures?
LANAP treatment is typically accomplished in two visits. Each of these visits will usually be around two hours, with one side of the mouth being treated per visit. The two treatments are scheduled within a week of one another.
During the first few days after your treatment, you make experience some mild soreness, or throbbing in the area. Mild pain medications can be used to help with the discomfort. You may notice some tissue around the teeth will appear discolored, and your bite may feel slightly different. Both of these are normal to experience immediately after the procedure.
- Do not brush or floss for the first 7 to 10 days following your treatment.
- We will provide instructions on your diet. You will typically be required to restrict yourself to liquids or mushy foods.
- Do not smoke, as this will have a negative impact on your gum treatment.
In the following months, you may experience shifting in your teeth, and your bite may need to be adjusted. Dr. Aerni may provide you with splits to help stabilize your teeth during this period. Please wear these splints as instructed in order to get the best results from your procedure. For the first year after LANAP treatment, we will usually suggest having your teeth professionally cleaned every three months, but this can vary from patient to patient. Please check with us for your specific treatment plan.
Below, we have provided a sample treatment plan to give you an idea of what to expect. Your exact plan may vary depending on your case.
Post-op Visit: Week 1
-Bite adjustments and healing management
-No brushing or flossing
-Soft diet for 3 to 10 days
Post-op Visit: Month 1
-Light cleaning and polishing
-Bite adjustments and healing management
-Wear splints each night and during the day (when possible)
-Brushing and flossing can resume
-Normal diet can resume
Post-op Visit: Month 4
-Periodontal maintenance
-Bite adjustments and healing management
Post-op Visit: Month 7 and Month 10
-Periodontal maintenance and checkup
-Bite adjustments and healing management
1 Year Evaluation
-X-rays and full periodontal charting
-Periodontal maintenance
-Bite adjustments and healing management
-Impressions for LANAP guard
-Identify areas needing possible re-treatment
-Discuss future treatment, such as recommended restorative, cosmetic, or orthodontic care
Am I a candidate for LANAP?
LANAP treatment is recommended for patients who have moderate-to-severe periodontal disease. It is also an ideal treatment for those who take medications such as blood thinners, as you will not be required to stop taking your medications for this procedure.
Can LANAP save dental implants?
Treatment with the PerioLase MVP-7 has been able to save dental implants that are failing by using a similar treatment known as the LAPIP™ protocol. This stands for Laser-Assisted Peri-Implant Procedure, and it allows for the implant to be stabilized while destroying the periodontal pathogens that are threatening it.
Although gingivitis and advanced periodontitis both affect your gums, they are two different health issues.
Your teeth are held in position by a number of things including bone tissue, ligaments, and your gums. If you do not properly care for your teeth, plaque can begin to form around your gums. Your gums begin to retreat and create “pockets.” These pockets allow for more bacteria to build up. This is gingivitis.
There are different severities of gingivitis, which is tested by measuring the deepness of the pockets around your teeth. You generally want pockets that are 1-3mm deep. Your pockets will be deeper if you have an infection.
Gingivitis, if left untreated, can form advanced periodontitis. Advanced periodontitis occurs when plaque and tartar infect your gums and begin to deteriorate the soft tissue that supports your teeth. If you do not treat advanced periodontitis, it can begin affecting the bone of your tooth. When this happens, the tooth is at risk of needing an extraction.
For minor plaque buildup, Dr. Aerni will be able to clean away the bacteria before it advances. If you are in a more advanced stage, a procedure called “scaling and root planing” will be done to clean around the gums and below your gums to remove tartar.
If you have developed gum disease—whether you have been properly caring for your teeth, or neglecting them—there is treatment available. How far your gum disease has advanced will determine what type of treatment your case demands. The most common form of treatment for gum disease is a deep cleaning. This type of cleaning will be necessary if you develop gum disease, as your regular cleanings will no longer properly clean your teeth and gum line.

Deep cleanings utilize special tools and techniques and include two steps: scaling and root planing.
The first step, scaling, removes tartar and plaque from the surface of your tooth and beneath your gum line.
The second step, root planing, is a process of carefully smoothing the surface of your tooth’s root to decrease inflammation, and shrink the pockets that have formed in your gums. If these pockets are left untreated, they will continue to allow plaque and tartar to build up under your gums and on your gum line.
Typically, a deep cleaning will require 2-4 visits to your dentist, and also may involve a local anesthetic during treatment.
Unfortunately, if your gum disease has developed too far, it cannot be fully cured, only treated. Gum disease is a systemic disease, very similar to diabetes or high blood pressure (HBP). After you have received a deep cleaning, it is important to continue treatment and schedule routine cleanings at Aerni Dental. If you do not receive routine cleanings, gum disease can cause tooth loss, loss of jaw bone, and lead to many other health problems.
What Is the Oral-Systemic Link?
It’s frequently said that the mouth is the gateway to the body. More and more, medical professionals have been discovering just how true this really is. This is referred to as the oral-systemic link.
Dentists are often the first to detect conditions such as Crohn’s disease, diabetes, or cancer because the early symptoms may first show up in the mouth. Going in the other direction, we’re learning more and more how what happens in your mouth affects the health of the rest of your body.
The brain has the blood-brain barrier which protects it from toxins in the blood. In our mouths, there is a barrier between our gums and teeth and the rest of our body as well. In the case of periodontal disease, this barrier can break down and may cause disease or other problems in the rest of the body. Previously, it was thought that bacteria were the main factor in this, but more recent research has been indicating that inflammation may play a bigger role.
While the details of this connection between oral health and the health of the rest of the body is still being explored, it’s becoming increasingly clear that treating the inflammation of periodontal disease can help with the treatment of other inflammatory conditions (and, in some cases, vice versa).
Diseases with oral connections
Some conditions with strong connections to oral health include:
Diabetes - Gum disease can make diabetes harder to control, and diabetes can exacerbate gum disease. We explore the topic in more detail on the linked page, here.
Heart disease and stroke - Conditions causing chronic inflammation, such as periodontal disease, have connections to the likelihood of heart disease and stroke. Read more about them on the page dedicated to the topic, here.
Respiratory disease - The bacteria that grow in the mouth can find its way into the lungs as well. Respiratory diseases, such as pneumonia, can be caused by the same bacteria responsible for periodontal disease.
Cancer - According to the American Academy of Periodontology, those with periodontal disease were more likely to develop cancer than those without:
-54% more likely to develop pancreatic cancer
-49% more likely to develop kidney cancer
-30% more likely to develop blood cancers
Other diseases that may be caused or complicated by oral infections include:
- IBS
- Breast cancer
- Prostate cancer
- Weight gain
- Alzheimer’s and dementia
- Low birth weight and premature birth
- Osteoporosis
- Rheumatoid arthritis
Some diseases can influence your oral health, as well, such as osteoporosis. Osteoporosis can lead to bone loss in the jaw which, in turn, can result in tooth loss, as there is no longer sufficient bone to support the teeth.
It’s critical to understand how important oral health truly is to our wellbeing, and to take it seriously in order to help prevent, or reduce the effects of other conditions.
Below, we’ll look at some of these conditions in a little more detail.
Colon Cancer
Gum disease provides a way for oral bacteria to find their way to other parts of the body. According to research done by Virginia tech, this bacteria may facilitate the spread of colon cancer and other types of cancer to other parts of the body.
The bacteria of interest in the study was Fusobacterium nucleatum, which is common in the mouth and has been found to invade tumors in the colon. Daniel Slade, Ph.D., an assistant professor in the Virginia Tech Department of Biochemistry explains the importance of the discovery that this type of bacteria may responsible for the spread of cancer in the body: “This is vital information because 90% of cancer-related deaths result from nonprimary tumors or sites that have metastasized to somewhere else in the body.”
In a 2017 study performed on mice, researchers found their first evidence that F nucleatum could be directly responsible for causes cancer in the colon to spread to the liver.
The research team has made examining the role this bacteria plays in the spread of cancer a focus on their treatment. Understanding the process by which this works can help medical experts find a way to inhibit the spread of cancer from one organ to another.
The team's latest study, “Fusobacterium Nucleatum Host-Cell Binding and Invasion Induces IL-8 and CXCL1 Secretion That Drives Colorectal Cancer Cell Migration” was published in Science Signaling.
While promising for future research into the treatment of cancer, these findings also further highlight the importance of treating gum disease, in order to minimize the presence of oral bacteria in the rest of the body.
Diabetes
The health of your mouth and the rest of your body are linked, and there’s an especially strong connection when it comes to diabetes and periodontal disease. For those who are suffering from diabetes, gum disease is often more likely and cases can be more severe.
How is diabetes linked to gum disease?
Diabetes is a disease that occurs when the amount of glucose, or blood sugar, in the body is too high. A hormone known as insulin is responsible for helping the cells in your body to use this glucose for energy. For those with diabetes, the body doesn’t produce enough insulin, so too much glucose stays in the bloodstream.
Inflammation in the mouth, such as the type responsible for periodontal disease, have an impact on the body’s ability to regulate blood sugar levels as well. This means that people with diabetes, whose bodies are already struggling with processing sugar, can find themselves having an even harder time if they are suffering from gum disease.
This link can go both ways, too, as high blood sugar levels provide an environment that can make gum infections more likely,
Heart Disease & Stroke
The potential links between periodontal disease and heart disease and stroke have been the subject of medical research in recent years. While a clear cause-and-effect relationship has yet to be established, findings lend a lot of credibility to the connection between oral inflammation and cardiovascular disease.
Researchers have found that chronic inflammation in the body is a major contributor to health problems in the body. This means that long-term inflammation, such as that in gum disease, may lead to narrowing or blockages in blood vessels—a situation that can lead to a heart attack or stroke.
In an article that looked at a number of related studies, it was found that having periodontal disease increases a person’s risk of cardiovascular disease by around 20%. One stroke expert reported that periodontal disease could make a person almost twice as likely to experience a stroke.
While research is still ongoing, what’s already been discovered should only put more emphasis on the need for a healthy mouth and gums.
If you have any concerns about the health of your mouth, or if you haven’t had a dental appointment in a while, make sure to get in touch to schedule your next visit.
Cancer
Links have been established between gum disease and many types of cancers.
Pancreatic Cancer
Studies performed at Brown University, Harvard, New York University, and others have looked into the link between gum disease and pancreatic cancer. Pancreatic cancer is extremely hard to detect and causes death within six months of diagnosis. It is approximated that pancreatic cancer is responsible for nearly 40,000 deaths per year in the US. So, what is the connection between gum disease and pancreatic cancer?
The connection comes from changes in the microbial mix in your mouth. Those who have porphyromonas gingivalis in their mouth were at a 59% higher risk of developing pancreatic cancer. In addition to prophyromonas gingivalis, those who had aggregatibacter actinomycetemcomitans were one 50% more likely to develop pancreatic cancer.
While the names may not mean much to the average person, the important thing to understand is that both of these types of bacteria have been tied to gum disease.
Unfortunately, the majority of Americans do not take proper care of their gums. It is reported that nearly half of American adults over the age of 30 have some form of periodontal disease. If you look at Americans over the age of 65, the percentage suffering from periodontal disease increases to 65%. Although not nearly as talked about, gum disease is almost 2.5 times more common than diabetes.
However, there is some good news! Gum disease responds extremely well to treatment and can easily be reversed after detected by your dentist.
Breast Cancer
A study done by the Federal University of Santa Maria Dental School in Brazil found that women with periodontitis are 2-3x more likely to develop breast cancer. In this instance, the researchers believe that breast cancer may be triggered due to systemic inflammation resulting from gum disease.
The study was based on 67 women who have been diagnosed with breast cancer and 134 controls from 2013 to 2015. It is important to remember that this study has not proven that gum disease causes breast cancer, but the findings do provide further support for the idea that oral health is vital to our overall wellbeing.
In the United States, for every 100,000 women, there are 124.9 new cases of breast cancer. Breast cancer continues to be studied, and this possible connection to oral health provides another avenue to be explored when learning to treat this type of cancer.
Esophageal Cancer
A 10-year study performed by NYU Langone Health’s Perlmutter Cancer Center has found that two types of bacteria that are present in individuals with gum disease can increase the chances of being affected by esophageal cancer.
The eight most common type of cancer in the world, esophageal cancer can be highly fatal and is the sixth most common cause of cancer-related deaths. In the US, it affects around 1 in 125 in men and 1 in 417 in women. The American Cancer Society says that currently, only around 20% of those diagnosed with this form of cancer will live for more than five years following diagnosis.
The study by NYU Langone found that bacteria associated with periodontal (gum) disease can find its way into the upper digestive tract, and in the case of one of the types of bacteria in the study, tannerella forsythia, its presence may increase the chances of this kind of cancer by 21%.
It is important to note that while the bacteria involved demonstrates a link between gum disease and esophageal cancer, it has not yet been proven that periodontal disease directly causes the cancer. However, the connection should be reason enough to reinforce the importance of proper oral hygiene and treatment of gum disease.
A November 2020 study found more evidence of connections between rheumatoid arthritis and periodontal (gum) disease.
What Is Rheumatoid Arthritis?
Rheumatoid arthritis a chronic inflammatory and autoimmune disease, which causes the immune system to mistakenly attack healthy cells of the body. It results in painful swelling of the affected tissues. While RA primarily affects the joints of the body, it can also damage the skin, lungs, heart, blood vessels, and eyes.
How Is Rheumatoid Arthritis Connected to Gum Disease?
Although there's still more to learn about whether or not one condition could be a cause of the other, past studies have found that people with RA are 8 times more likely to develop gum disease than those without RA. It's also been found that the type of bacteria that causes periodontal disease, porphyromonas gingivalis, can lead to an earlier onset of RA and make it more severe.
Connections With Cardiovascular Disease
People with rheumatoid arthritis also face elevated risks for cardiovascular disease, which itself has links to periodontal disease.
The November 2020 study in Arthritis & Rheumatology found that a pathogen related to periodontal disease, called aggregatibacter actinomycetemcomitans, "had the strongest associations with atherosclerosis in the patients with rheumatoid arthritis that we studied," according to Jon T. Giles, MD, MPH, of Columbia University.
While research into the connections between periodontal disease and other diseases continues, this should further reinforce the importance of a healthy mouth. Preventing or treating gum disease may very well prevent or lessen the impact of ailments such as rheumatoid arthritis.
Gum Disease and Reproductive Health
It can't be overstated how much the health of the body is connected to oral health. Research has found that gum health is even linked to sexual and reproductive health.
The plaque that develops as a biofilm in our mouths is made up of bacteria, including these:
- Porphyromonas ginigvalis
- Tannerela forsynthia
- Prevotella intermedia
- Aggregatibacter actinimucentemcomitans
- Treponema denticola
Periodontal disease allows these pathogens, which originate in the mouth, to be introduced into the bloodstream. The presence of some of these types of bacteria in the bloodstream is where many of the links between oral health of various other ailments have been discovered. And it isn't just the bacteria itself, but the resulting inflammatory response and waste products of the bacteria that can cause problems.
Pregnancy and Oral Health
In the case of pregnancy, it's believed that these pathogens can cause negative outcomes such as low birth weight or premature birth. A few studies have suggested that women suffering from chronic periodontitis may be 4 to 7 times more likely to give birth prematurely.
Women who become pregnant should be aware that hormonal changes make them more susceptible to getting gum disease as well. Gum disease has been linked with preeclampsia, a condition which can damage internal organs such as the kidneys and liver of both the baby and the mother.
Fertility and Periodontal Disease
Along with the impacts on pregnancy, studies have found that gum disease can play a role in fertility, with both male and female fertility being impacted.
One study in Australia found that women with periodontal disease may require two more months to conceive than those without. In men, the bacteria related to gum disease lead to low sperm count, poor sperm motility. There appears to be a connection with erectile dysfunction as well, with men who have gum disease being more likely to suffer from ED.
According to the National Institutes of Aging, the bacteria responsible for periodontal disease are also associated with the development of dementia (particularly vascular dementia) and Alzheimer’s disease.
We frequently emphasize the importance of oral health and treatment of periodontal/gum disease, as this infection of the tissues surrounding the gums allows bacteria from the mouth to enter the bloodstream and affect other parts of the body.
Using data from the National Health and Nutrition Examination Survey along with blood tests, the National Institutes of Aging researchers looked at a group of more than 6,000 people to find if the oral bacteria in gum disease could be linked with diagnoses of dementia.
They looked for nineteen different types of oral bacteria, including Porphyromonas gingivalis, which is the most typical type of bacteria found in gum disease. In those who are afflicted by Alzheimer’s, it’s been found that beta-amyloid proteins can clump together to form plaques. A previous study has suggested that these plaques may actually be produced in the body as a response to Porphyromonas gingivalis.
One of the findings was that older adults with gum disease at the start of the study were more likely to develop Alzheimer’s during the course of the study than those who did not have signs of gum infections.
While it appears to be clear that there are connections between dementia and the bacteria found in periodontal disease, researchers are looking into more long-term studies to learn more about this association. The current findings suggest that gum disease may precede cases of dementia, but it’s also known that dementia makes it harder for patients to properly care for their teeth and gums. Further research needs to be done into whether or not treatment of infections of gingivalis can have an impact on Alzheimer’s disease.
What is Osteoporosis?
Osteoporosis is a disease of the bones involving the reduction of bone mineral density and mass. These changes in bones can cause them to become more fragile and put them at greater risk of breaks or fractures.
Considered a “silent” illness because of the subtlety of, or lack of, any noticeable symptoms, many people who suffer from osteoporosis are not even aware that they have it until they break a bone. However, osteoporosis is the leading cause of bone fractures in older men and women.
How Is Osteoporosis Related to Oral Health?
When considering osteoporosis in the context of oral health, the potential connection to periodontal disease is that one that interests researchers. Periodontal disease, or gum disease, if left unchecked, can lead to the loss of the bone and connective tissues that hold teeth in place. Since both diseases can have an impact on bone, the interaction between the two is something that needs to be better understood.
Research is currently inconclusive when it comes to whether or not having osteoporosis can lead to an increase in the chances of developing gum disease, however, for those who are suffering from gum disease and osteoporosis, data indicates that there is a higher chance of seeing deterioration in the alveolar bone which hold teeth in place.
For this reason, it is a good idea to let your dentist know if you have osteoporosis, especially if you are currently being treated for, or at risk of developing gum disease, as the condition may cause periodontal disease to progress more quickly.
What Are the Symptoms of Osteoporosis?
In the US, it’s estimated that about 54 million people have osteoporosis. Bone mineral density tests ordered by your healthcare provider are the typical way that the disease is diagnosed. There aren’t any overt symptoms to look for, which is why, for many, bone fractures are the most obvious indicator, however, some things to watch out for include:
- Reduction in height
- Change in posture
- Reduction in lung capacity
- Pain in the lower back.
How Can Osteoporosis Be Avoided?
Recommended steps to take to lower your chances of developing osteoporosis include:
- Getting regular exercise
- Eating a healthy diet rich in vitamin D and calcium
- Avoiding smoking
- Avoiding excessive alcohol use
Respiratory disease can also be referred to as pulmonary disease or lung disorder. These are conditions that affect the lungs and have an impact on breathing. Some forms of respiratory disease may be caused by air pollution or tobacco smoking, while others are the result of infection.
How is respiratory disease connected with gum disease?
We normally think of periodontal disease as a localized infection of the gums and connective tissues in the mouth, but researchers are finding more evidence to link it to respiratory diseases, either playing a possible role in contraction of the illness or in increasing its severity.
Respiratory diseases with links to periodontal disease include:
- Chronic obstructive pulmonary disease (COPD)
- Pneumonia
- Bronchitis
- Emphysema
Gum disease and pneumonia
Pneumonia is a type of inflammation of the lungs caused by infection by bacteria, viruses, or fungus, though bacterial infections are the most common. The disease results from these infections making it to the lower part of the airway.
In healthy people, the body has defense mechanisms which prevent bacteria from the mouth from being able to reach places far into the lungs, but there are instances where this can be impaired, such as malnutrition, diabetes, or smoking.
In an examination of patients with pneumonia undergoing care in an ICU, it was found that patients who had dental plaque upon their admission to the ICU, or within the first five days of their stay, were 10 times as likely to develop pneumonia as those who were plaque-free.
In a two-year study of nursing home patients, one group was given routine toothbrushing by a caregiver as well as weekly professional care for plaque and tartar. At the end of the study, it was found that the group receiving oral care had fewer cases of pneumonia (11% vs 19%) and lower instances of pneumonia-related mortality (8% vs 16%).